Struggling to Relax? A Compassionate Guide Using Compassion Focused Therapy
- Dr Tiffany Leung

- Dec 16, 2025
- 13 min read
Updated: Dec 24, 2025

Introduction
Many people who appear capable, resilient, and composed on the outside quietly struggle to slow down. Even when life is full and responsibilities are met, there can be an undercurrent of pressure, a sense that you should be achieving more, managing better, or holding yourself to a higher standard.
You may recognise a familiar voice inside, one that pushes you to keep going or warns that resting too early means you are slipping. This is especially common among people who have carried long-term stress, high expectations, or cultural messages about what it means to be hardworking, responsible, or “good enough.”
For some, this pattern is rooted in childhood or cultural environments that value endurance and achievement.
For many women, femmes, or sexually fluid individuals navigating professional hierarchies, the pressure to stay composed and continually “prove yourself” can make rest feel risky, as if slowing down might be misinterpreted as not being capable enough.
For others, it reflects lived experiences of migration, identity, or being one of the few in a professional space, where vigilance became a way of maintaining belonging and opportunity.
And for many neurodivergent individuals, the constant management of sensory demands, masking, or adapting to environments not made for them keeps the nervous system perpetually alert.

In therapy, I often hear people say, “I cannot switch off,” or “Rest feels unfamiliar to me.”
These are not signs of failure. They are signs that your emotional systems have learned to survive by staying active, vigilant, or striving.
The Compassion Focused Therapy (CFT) model, developed by Professor Paul Gilbert (Gilbert, 2010; Gilbert, 2014), offers a gentle and insightful way to understand these experiences. It helps you understand why rest feels difficult, why self-criticism is persistent, and how you can recondition your nervous system to experience safety, steadiness, and genuine ease.
At a Glance: What You Will Learn
Why rest feels difficult
How threat and drive become dominant through stress, identity pressures, trauma, or high-achievement environments.
The three emotional systems in Compassion Focused Therapy
Threat protects, drive pushes, and soothing helps you feel safe and grounded.
How trauma and neurodivergence shape your nervous system
Chronic demands narrow the window of tolerance and make rest feel unfamiliar.
Practical ways to grow your soothing system
Gentle, sensory-based, culturally meaningful strategies that help you find steadiness without pressure.
This guide is for anyone who finds it hard to relax, even when life looks successful from the outside. It weaves psychological insight, cultural understanding, and compassionate practice to help you reconnect with a calmer, more caring version of yourself.

Why Rest Feels Difficult: A Psychological View
Difficulty relaxing is seldom about poor discipline or a lack of willpower. More often, it reflects a body that has learned to stay alert, productive, or watchful in order to cope with life.
When you have spent years meeting expectations, navigating uncertain environments, or managing pressure related to gender, culture, class, or identity, the nervous system adapts. Rest becomes unfamiliar because your body has been living in a state of readiness.
You may have grown up in a home where slowing down was discouraged or misunderstood. You may have lived through periods of instability, conflict, or stress where relaxing simply did not feel safe.
There are also quieter pressures.
You may move through workplaces where you feel watched or evaluated.
You may have absorbed cultural messages about endurance and responsibility.
You may know the tension of needing to appear competent, composed, or “on top of things,” especially in spaces where you have felt underestimated.
Gendered expectations deepen this instinct. People who have carried emotional labour, held harmony, or sustained high performance often struggle to give themselves permission to pause.
And for those managing neurodivergent demands: sensory overload, transitions, masking, the body may not recognise cues for settling at all.
When we look closely, difficulty relaxing is not a flaw. It is the natural outcome of systems that have worked hard to protect you.
Understanding these patterns gently opens the door to change.
Introducing the Compassion Focused Therapy Model
Compassion Focused Therapy (CFT) offers a simple but powerful way to understand why you move through the world the way you do.
Instead of framing emotional reactions as weaknesses, CFT helps you explore the three systems that influence how you respond to stress, responsibility, and safety.
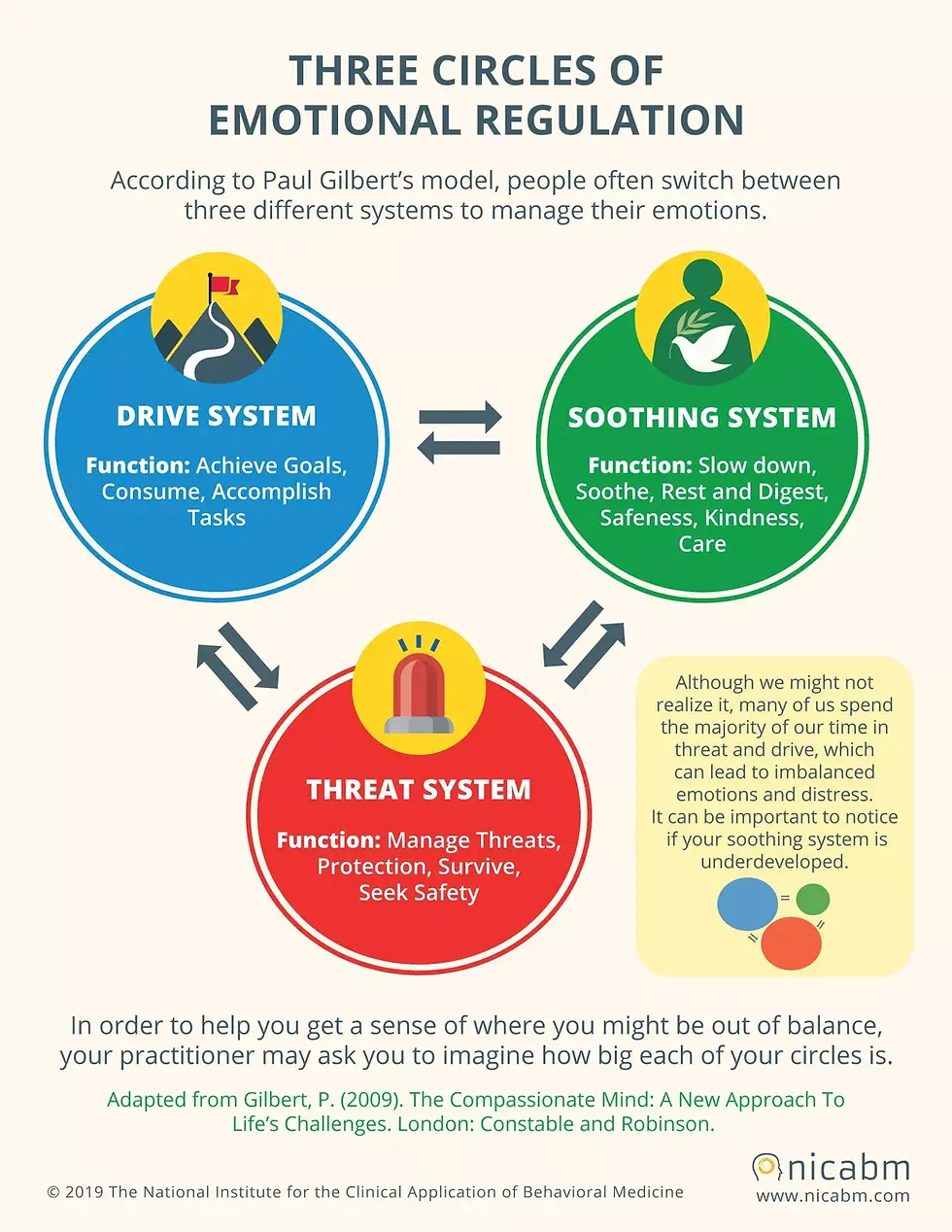
The Three Emotional Systems in CFT
The Threat System: Protection
This system activates when you sense danger, criticism, rejection, or uncertainty.
It brings anxiety, tension, vigilance, self-criticism.
If you have lived with trauma, chronic pressure, bias, or scrutiny, this system becomes highly sensitive: quick to activate, slow to settle.
The Drive System: Achievement
This system motivates you to pursue goals and meet demands.
It is essential for ambition and growth.
But when you have learned that your worth depends on performance or composure, particularly in demanding or hierarchical environments, the drive system becomes dominant. It keeps pushing even when the body asks for rest.
The Soothing System: Safety and Rest
This system allows you to feel grounded, safe, connected, and calm.
It supports rest, play, compassion, and emotional steadiness.
For many people, soothing is underdeveloped not because of personal failure, but because life never provided enough opportunities for safety, comfort, and unconditional support.

The Core Truth of CFT
Your wellbeing depends on balance between all three systems.
Not eliminating threat.
Not suppressing drive.
But allowing soothing to take its rightful place.
Each system has a purpose: threat protects, drive helps you grow and achieve, and soothing allows you to recover, connect, and feel safe enough to live, not just endure.
When threat and drive dominate, rest becomes unfamiliar, not because you are failing, but because your emotional systems are imbalanced.
How Trauma and Identity Shape the Nervous System
Trauma-informed psychology helps explain why threat and drive can become dominant and why soothing feels difficult.
The nervous system learns through experience
If you have lived through unpredictability, conflict, pressure, or survival, the body may continue to behave as if danger is near, even when life is calmer.
This is a protective adaptation, not a choice.
The window of tolerance narrows under chronic stress
Window of tolerance refers to the zone where your emotional system can handle stress without becoming overwhelmed or shutting down.
When you live outside this window for a long time, through chronic stress, caregiving, achievement pressure, workplace bias, cultural expectations, or identity-based challenges, your threat system becomes more reactive, and your drive system works harder to compensate.

Felt safety matters
Feeling safe is not the same as being safe.
Many people struggle to sense safety even during moments of calm.
Identity and hierarchy shape nervous system patterns
If you have been “the only one like me” in academic, corporate, or high-stakes settings, or you have been underestimated, judged more harshly, or required to perform flawlessly, vigilance becomes normal.
Rest can feel less like recovery and more like a risk.
This is where CFT becomes deeply supportive.
The soothing system grows through gentleness, repetition, and emotional safety, not pressure.
Did you know?
Many people assume that “relaxing” is a decision. But from the perspective of the nervous system, it is often more like a bodily capacity. When long-term stress keeps the threat system highly activated, it may not be that you do not want to relax, but that your body temporarily struggles to recognise “this moment is safe.” The soothing system does not grow through force. It more often returns gradually through experiences of being understood, held, and given permission.
Why Your Soothing System May Feel Underdeveloped
Even though soothing is essential for wellbeing, many people struggle to access it. Not because anything is wrong with you, but because the soothing system has been overshadowed by other systems working overtime.
1. Threat and drive have been active for too long
When you spend years scanning for danger, meeting expectations, or proving yourself, even for understandable reasons, soothing has fewer opportunities to grow.
2. Early environments may not have modelled soothing
If you grew up encouraged to be strong, self-sufficient, composed, or emotionally contained, soothing may have felt optional or indulgent.
In these environments, drive and threat were often rewarded, soothing may even have been seen as unhelpful.
3. Workplaces reinforce vigilance
High-pressure, biased, or hierarchical environments reward productivity and composure over ease.
The drive system thus stays switched on. And when you navigate environments where you have been underestimated, excluded, or judged more harshly, the threat system is even more easily dominating.
4. Trauma keeps the body prepared
Past experiences also play a powerful role. If life has involved trauma, instability, sudden change, or prolonged stress, the nervous system learns to stay ready.
Even in stability, the nervous system may not trust rest.
You may read more in my other article about what trauma is and its impact on our wellbeing: What is Trauma? A Psychologist's Guide to Definition, Signs & Healing
5. Neurodivergent sensory needs
Daily sensory demands, transitions, and masking require constant energy, a kind of baseline vigilance.
The nervous system does not get many chances to down-shift into soothing.
Rest may need more predictability, structure, or sensory adjustments than others realise.
6. Identity and relational pressures intensify activation
Gendered expectations, emotional labour, class mobility, and cultural or professional hierarchies amplify threat and drive.
Over time, the body learns that staying alert is necessary, while softening carries risk: risk of being judged, falling behind, or losing credibility.
Key insight
When we see this clearly, the soothing system’s quiet voice makes perfect sense.
Your soothing system is not underdeveloped because you failed.
It is quieter because your other systems have worked hard to protect you.

Once you can see how these patterns formed, you do not have to fight them.
You can begin to shift them with gentleness, using skills that help your nervous system feel safer, not more pressured.
Why High Achievers and People in Cross Cultural Contexts Often Find It Harder to Relax
Some people find it hard to relax, not because they lack self-discipline, but because they have become used to keeping themselves in a state of being “available” and ready.
When you move through high-achievement environments with clear hierarchies, being evaluated and compared can leave your body feeling as if it is constantly on standby.
Cross-cultural and migration contexts also deepen this, the ongoing adaptation and calibration to language, rules, social nuance, and unspoken expectations can keep you scanning without noticing.
Gendered expectations and emotional labour can make it easier to place your own needs last.
And if you also live with neurodivergent sensory load and masking, it can become even harder for the body to downshift naturally.
CFT reminds us that this is not a flaw. It is a form of protection that was once necessary. The focus is to help the soothing system slowly return to its rightful place, so that rest becomes more accessible.
Building the Soothing System: What Actually Helps
Many people I work with worry that they “do not know how to rest,” or that something is wrong with them for struggling.
The question is not:
“How do I force myself to relax?”
but
“How do I rebalance these systems so soothing becomes possible again?”
Rebuilding the soothing system is not about suppressing drive or threat. It is about helping all three systems work together.
1. Relearning the Physiology of Rest
The body needs signals, not instructions.
Instead of just 'telling' your body to calm down, use sensory cues that signal safety:
warm temperature
slow exhalations
grounding through touch
gentle movement or rhythm
soft sensory input
For neurodivergent individuals, these cues may need more structure or predictability, such as consistent lighting, noise-cancelling headphones, weighted blankets, or having control over when and how transitions happen.
2. Creating Safety Before Rest
For many, rest has been judged, questioned, or interpreted through roles they have had to carry.
Prepare the environment or transitions so the body does not feel abruptly switched off:
adjusting lighting, noise, temperature
limiting demands or interruptions
using transitions, so the body shifts state gradually
having a grounding object such as weighted blanket or sensory support
allowing yourself permission to pause without earning it
3. Compassionate Inner Dialogue
Shift your internal tone from self-criticism to nurturing language.
Instead of:
“I should be relaxing.”
“Why am I like this?”
“I need to stop overreacting.”
You might try:
“This is unfamiliar for me, and I am learning.”
“My body is doing what it was taught to do to protect me.”
“I can take this slowly.”
This is the same internal language we would offer a friend we care about.
4. Personal and Cultural Soothing Practices
Soothing is deeply personal, not one-size-fits-all.
Stillness, quiet movement, ritual, music, warmth, prayer, artistry...
Choose what genuinely feels safe and meaningful to you, not through what others promote as relaxing.
5. Slow, Gentle Repetition
Soothing grows through consistency, not intensity.
A few seconds of grounding repeated daily changes more than a single long rest. A brief acknowledgement of how your body feels can begin to shift your internal state.
Your soothing system is like a muscle. If it has not been exercised, it simply needs time, practice, and kindness. Each moment of warmth teaches your nervous system that safety is possible.

How to Re-Communicate with Your Threat and Drive Systems
Before you can rest, it can help to shift the way you relate to the parts of you that have been working so hard to protect and motivate you.
1. Understanding the Threat System (with Compassion)
The threat system reacts quickly. What we often call the “inner critic” is usually a threat-system voice trying to protect us. It may say things like:
“Be careful.”
“Do not let your guard down.”
“You need to do better.”
The “inner critic” is often a protective voice shaped by fear.
Fear of being hurt.
Fear of being judged.
Fear of losing stability or belonging.
Re-communicating with the threat system starts with acknowledging its intention, even when its method is painful. Try:
“I see you are trying to keep me safe.”
“You learned this tone because the world has been hard.”
“You are protecting me, even though it feels difficult.”
2. Understanding the Drive System Without Shame
Many clients describe feeling guilty for stopping, struggling with rest unless everything is finished, staying productive to avoid being judged or falling behind.
Your drive system has carried you through demanding environments.
Try to acknowledge how hard your drive system has worked for you:
“You have kept me going when life was demanding.”
“You helped me survive environments that expected perfection.”
“You do not have to push as hard in this moment.”
3. Helping the systems work together
Invite soothing into the conversation rather than forcing threat or drive to turn off:
“I know you are alert because you care about my safety.”
“We are not in danger right now. We can pause together.”
“We can move at a pace that does not exhaust us.”
“There is room for warmth as well as achievement.”
4. Allowing The Trio to Co-Exist
Threat warns.
Drive motivates.
Soothing steadies.
All three have a place.
When these systems learn to relate to each other differently, the whole emotional landscape becomes steadier. We are no longer pulled by urgency or pushed by fear. Instead, we develop an inner environment where protection, motivation, and calm can coexist.
When you feel overwhelmed, ask:
“Which system is speaking right now, and what is it trying to protect me from? What does it need?”
Awareness creates choice. Choice builds soothing.

A More Compassionate Way to Reconnect with Yourself
When you understand the emotional systems shaping your experience, struggling to rest begins to make sense.
It is not laziness or resistance.
It is protection.
The soothing system grows through permission, not pressure.
Through warmth, not willpower.
Through gentle repetition, not discipline.
This does not fix everything, but it shifts you into a more compassionate relationship with yourself: one that honours the pressures you have faced and the resilience you have built.
You deserve a life that is not only productive, but also steady, spacious, and kind.

If You Are Exploring This Work
If you recognise these patterns in yourself: the constant striving, the quiet pressure to hold everything together, or the difficulty switching off even when you are exhausted, therapy can offer a steady and thoughtful space to understand these experiences.
It can be one of the few spaces in your week where you do not have to perform or hold everything together, where the focus is on understanding you rather than evaluating you.
Working together, we can explore how your emotional systems have been protecting you, and how to restore balance, safety, and genuine ease.
You are more than welcome to continue reading:
Frequently Asked Questions
Why do I feel anxious as soon as I try to rest?
For many people, anxiety during rest is not a sign that you are “bad at relaxing.” It can be a sign that your threat system has learned to associate slowing down with risk. If you have relied on vigilance and productivity to stay safe, capable, or accepted, rest can feel unfamiliar, even destabilising. Your nervous system may need gradual transitions and signals of safety before calm becomes available.
Is self criticism linked to difficulty relaxing?
Often, yes. Self criticism is frequently the voice of the threat system rather than a truthful assessment of your worth. It can develop as an attempt to prevent mistakes, rejection, or judgement, especially in environments where you had to perform well to be safe or respected. When this internal tone is intense, the soothing system has less room to emerge. CFT helps you understand self criticism as protection, and supports a shift towards a steadier, kinder inner relationship.
Who is Compassion Focused Therapy (CFT) helpful for?
CFT can be particularly supportive if you experience persistent self criticism, feel driven to keep achieving, struggle to switch off, or find rest unfamiliar. It is often helpful for people living with long term stress, high expectations, identity based pressures, or the effects of trauma. Rather than aiming to eliminate threat or ambition, CFT focuses on restoring balance between systems, so that safety, steadiness, and genuine ease become more accessible.
How can neurodivergent people access the soothing system more easily?
For many neurodivergent individuals, soothing is less about mindset and more about nervous system conditions. Sensory overload, transitions, masking, and chronic adaptation can keep the body activated. Soothing often becomes more available when there is predictability, environmental support, and respect for sensory needs, such as reducing sensory demands, pacing transitions, and building in stabilising cues. In this sense, soothing can be understood as designing life in a way that your nervous system can trust.
What is the window of tolerance, and how does it relate to trauma?
The window of tolerance describes the range in which your nervous system can stay regulated while experiencing stress. When you are within this window, you can feel emotion without becoming overwhelmed or shutting down. Trauma and chronic stress can narrow this window, making the threat system more reactive and making calm harder to access, even when life is objectively safer. Building the soothing system can gradually expand this window, supporting greater emotional steadiness and a more reliable sense of felt safety.
Disclaimer
This article is for reflection and education only.
It is not a substitute for therapy, diagnosis, or personalised psychological advice.
If you are considering therapy, you are welcome to seek support from a qualified mental health professional who can explore your individual needs with you.
Struggling to Relax? A Compassionate Guide Using Compassion Focused Therapy
Struggling to Relax? A Compassionate Guide Using Compassion Focused Therapy




Comments